(Jakarta) – The Indonesian government has taken important steps to end the practice of shackling people with mental health conditions, Human Rights Watch said today. But many people remain locked up in institutions instead of being able to live in the community.
The number of people with psychosocial disabilities (mental health conditions) who are shackled or locked up in confined spaces dropped from nearly 18,800, the last reported figure, to about 12,800 in July 2018, according to Indonesian government data. The change resulted in part from community outreach to over 16.2 million households.
“The Indonesian government has made a serious effort to tackle the practice of shackling and the lack of community-based mental health services,” said Kriti Sharma, senior disability rights researcher at Human Rights Watch. “But with little oversight, thousands of people with disabilities remain in chains or locked up in institutions across Indonesia.”
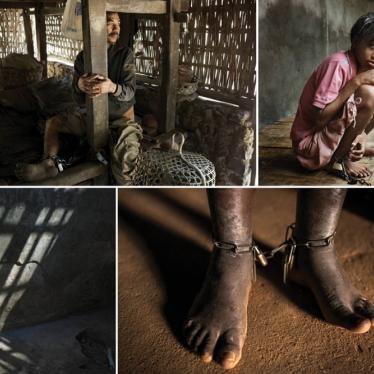
Human Rights Watch found in its 2016 report, “Living in Hell: Abuses against People with Psychosocial Disabilities in Indonesia,” that thousands of people with psychosocial disabilities were shackled and many were forcibly detained in overcrowded and unsanitary institutions. The practice persisted despite a 1977 government ban on shackling because of stigma and the lack of community-based support or mental health services.
Since then, Human Rights Watch has visited Indonesia five times to monitor government progress in addressing the problem. Human Rights Watch conducted 19 interviews with people with psychosocial disabilities and 48 interviews with family members, caregivers and institution staff, health professionals, disability rights advocates, and government officials across Jakarta, Bekasi, Bogor, Cianjur, Brebes, and Tegal.
Over the past two and a half years, the government has taken promising steps to address shackling. In April 2016, Health Minister Nila Moeloek made a commitment to make mental health medication available in community health centers across the country.
By January 2017, the Health Ministry rolled out Program Indonesia Sehat dengan Pendekatan Keluarga (Healthy Indonesia Program with Family Approach), a community outreach program in which health workers use a “family-based approach,” going house to house to collect data, raise awareness, and provide services relating to 12 measures of family health, including mental health.
As of September 2018, the program had reached 16.2 million – roughly 25 percent – of Indonesian households. The data collected indicates, however, that only 16 percent of people with psychosocial disabilities surveyed have access to mental health services.
A 52-year-old woman with a psychosocial disability was one of many rescued by community health workers in Cijeruk, Bogor. “We locked her in her room for five years,” her sister said. “She would sleep on the floor; she couldn’t walk because her muscles had stopped working. We gave her a bucket to urinate and defecate in. It was very smelly. It made me very sad.”
The family felt they had no alternative but to lock her up. But after a visit and help from outreach workers, her sister said, the family released her from her room in February 2017 and she is now receiving services in the community.
“Integrating mental health into primary health care is crucial but it’s not enough,” Sharma said. “To eliminate shackling, the government needs to educate the public about mental health and provide people with psychosocial disabilities with services that extend beyond medication, including access to education, housing, and employment.”
Human Rights Watch found that people with psychosocial disabilities continue to be arbitrarily detained in faith healing centers, social care institutions, and mental hospitals. In the absence of regular monitoring, little has changed in faith healing centers, where people are shackled, abused, and forced to take alternative “treatments” such as herbal concoctions, vigorous massages by traditional healers, and forced listening to Quranic recitations. In private institutions, people with psychosocial disabilities routinely face abuse including physical and sexual violence, involuntary treatment, restraints, and forced seclusion.
At Yayasan Galuh Rehabilitation Center in Bekasi, a woman in her mid-thirties with a psychosocial disability, said: “I used to be chained at home. My family tricked me into coming here. They told me my mother had passed away and they were taking me to her funeral. Instead they brought me here. I was locked in an isolation room for four weeks because I got into a fight.”
The Ombudsman, National Human Rights Commission, and National Commission on Violence against Women should immediately order inspections and regular monitoring of all government and private institutions and take appropriate action against abusive facilities, Human Rights Watch said. The Social Affairs Ministry also has a responsibility to regulate private institutions and ensure that it is not inadvertently enabling abusive practices.
“Despite the progress, the government has a long way to go to end abuse in institutions,” Sharma said. “The Social Affairs Ministry needs to adopt a deinstitutionalization policy that moves away from warehousing people in institutions and supports independent living in the community.”
Government Progress Against Shackling
In 2017, the Indonesian ministers of home affairs, health, and social affairs, the chief of the National Police, and the Indonesian Health Insurance Organization signed a memorandum of understanding to work together to comprehensively carry out the 1977 ban on shackling. Both the Social Affairs and Health Ministries have campaigns to end shackling by 2018 and 2019 respectively.
They carried out awareness-raising activities and provided training for provincial-level staff across the country. Human Rights Watch found that many community health centers have also created their own initiatives to eliminate shackling at a local level. Puskesmas Banjarsari in Ciawi, in one example, has started a text message hotline called “care about shackling” to encourage people to report shackling cases.
Human Rights Watch returned to many communities where it had documented shackling to find that people had been released and were living in the community. When Human Rights Watch first visited Sodikin, a 34-year-old man with a psychosocial disability, in 2014, he was locked up in a tiny shed outside the family home in Cianjur, West Java. The family initially tried to get him medical care but the local health center didn’t have mental health medication and the hospital was too far. Sodikin spent more than eight years shackled in the shed, given his meals through a small hole in the shed, before being released with the help of a local nongovernmental organization in May 2016.
Sodikin’s brother-in-law said: “Sodikin had become very thin. When he was released, his legs were stiff and he couldn’t even stand up or walk so I had to carry him.” Sodikin spent six months recovering in a nongovernmental organization-run shelter before he could come home. Sodikin now works at a clothing factory stitching buttons onto boys’ school uniforms. “We were so happy to have him living in the family home again,” his brother-in-law said. “We never thought he’d recover. His father used to see him as a burden, and now he’s the main bread winner supporting the family.”
According to the Indonesian Mental Health Directorate, the number of people being shackled or locked up in confined spaces across 32 provinces (excluding Papua and West Papua) decreased from 13,528 in December 2017 to 12,832 in July 2018. However, documenting shackling is difficult as it often occurs in remote areas, and families are reluctant to speak due to the shame and stigma around mental health conditions. In addition, people who are rescued sometimes end up in shackles again because of the dearth of community support services.
Human Rights Watch found that one of the risks with government efforts to eradicate shackling is that some people who are released end up in mental hospitals where they could be arbitrarily detained or treated without their consent.
A mental health nurse at Bogor Mental Hospital said: “When we intervene in a shackling case, patients don’t always want to come to the hospital or are in no state to communicate so the family member is the decision-maker.” However, informed consent of the affected individual is a bedrock principle of medical ethics and international human rights law, and not allowing people with psychosocial disabilities to make their own medical decisions violates their rights.
Following his March 2017 visit, the UN’s expert on health, Dainius Puras, urged the Indonesian government to “scale-up” its campaign against shackling but to ensure that it is not “replaced by other forms of restraints and confinement which violate human rights.”
In partnership with the Indonesian Psychiatric Association and nongovernmental groups, the World Health Organization (WHO) is training psychiatrists, doctors, nurses, social workers, government officials, and disability rights advocates in Indonesia in its Quality Rights initiative, which aims to provide alternatives to coercive practices such as involuntary treatment, seclusion, and restraints in mental hospitals and social care institutions.
In May 2018, it began training on the internet for 61 people from 19 different provinces, and in November it will provide in-person training for 80 people. While the WHO training is an important effort in eliminating coercion in hospitals and institutions, the government should amend the 2014 Mental Health Act to ensure that people with psychosocial disabilities cannot be arbitrarily detained against their will, in line with its obligations under the international Convention on the Rights of Persons with Disabilities.
Government Efforts on Mental Health
The government has shown its commitment to making mental health a priority by including it as one of the 12 indicators in its national community health program, the Program Indonesia Sehat dengan Pendekatan Keluarga (Healthy Indonesia Program with Family Approach). The program is an ambitious government initiative that seeks to ensure that even the most rural, isolated, and reluctant communities get access to health services. The program’s home visits are critically important because they eliminate the need for family members to take time off from work and spend money to travel to health centers.
For the program’s nationwide rollout, the Health Ministry trained 25,000 master trainers to train five staff members in every community health center across Indonesia. Relying on community workers such as midwives or social workers to deliver basic mental health services has meant that the shortage of trained mental health professionals is no longer a barrier. The trained staff in turn educate additional health center staff about the program and mental health. By the end of 2018, 6,205 community health centers will be operating the program. The government’s target is to ensure full coverage of over 65 million households in Indonesia through all 9,909 community health centers by the end of 2019.
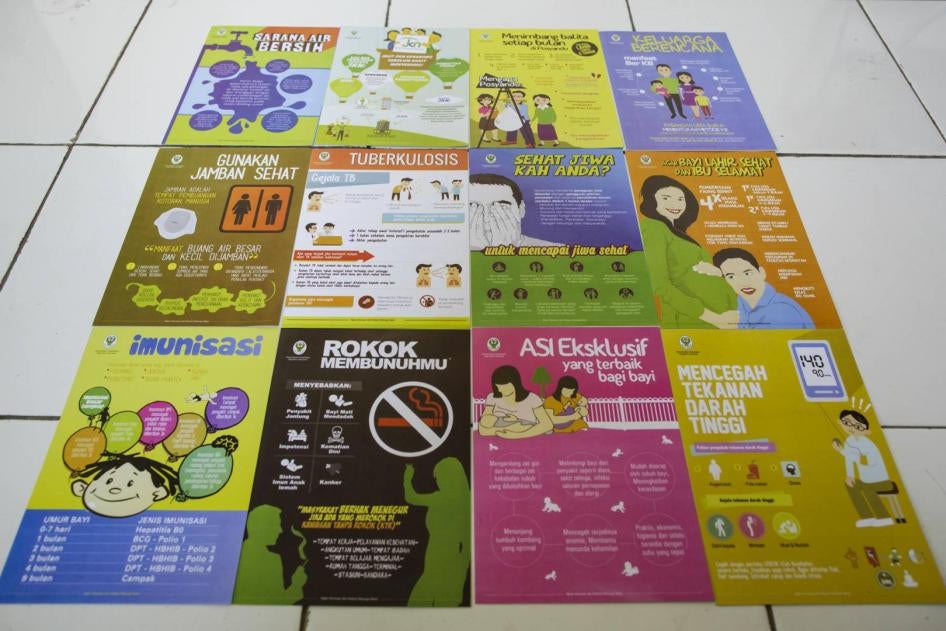
The program’s innovative “family-based approach” looks at 12 measures that together reveal family health – access to clean water, hypertension, tuberculosis, smoking, family planning, access to government health insurance, maternal health, child nutrition, immunization, breast feeding, sanitation, and mental health. If a family fairs poorly on even one indicator, then it is identified as needing assistance. This system effectively gives mental health the same importance as all other indicators, and ensures that community health workers provide immediate and ongoing mental health services to meet their target of 100 percent coverage.
Since the program involves home visits, it becomes easier for community health workers to detect cases of shackling and facilitate the release of shackled people. Dr. Tina Yustiniarsih, a community health center doctor, said that she intervened to rescue Asep, a 34-year-old man shackled for three years in Banjarwangi village in Ciawi:
We found Asep chained in a dilapidated abandoned house. The chain around his waist was so heavy, it took us 15 minutes to cut through it with a saw. I counseled the family, told them that someone with a mental health condition is the same as we are, they have human rights. We also briefed the entire village to make sure everyone knew that people with a mental health condition should not be shackled.
Asep’s sister said, “I felt sad seeing him in shackles. I agreed immediately to him being released, I wanted him to get better. If the health team hadn’t come, we would never have released him.” She didn’t know about the benefits available with the national health insurance card and available services at the hospital.
Asep said: “I felt cramped and rigid in shackles. I don’t remember exactly what happened but I was happy when I was freed.”
During house visits, the community health worker collects data, educates the family about mental health, provides counseling, and helps them get a national health insurance card for free or subsidized health services. In addition, the person with a psychosocial disability and their family can visit the community health center for one-on-one counseling with a doctor or nurse, they can get medication, and they can participate in occupational therapy or other activities. In some cases, the health center facilitates formation of peer support groups through the messaging application WhatsApp, links people to training on how to start a small business, and helps them get funding to start the business.
Siti, a 39-year-old woman with a psychosocial disability living in Ciawi, Bogor said that, “[The staff] are quite helpful. I am happy they gave me capital funding of Rp. 2,800,000 [US$190] to start my hair salon. This way I can earn some income.”
Siti’s sister said that their lives have changed after getting the program’s support:
Before, we had to travel all the way to the mental hospital to get medication. Sometimes we didn’t have time to go or the transport was too expensive. Since we got help from the community health center, Siti’s condition is much better. In addition to medication, the center provided counseling, connected us to support groups, and is facilitating support for her business. My dream for Siti is that she is completely independent.
While the program has significant potential to provide easy access to voluntary community-based mental health services, it is still in a nascent stage. Even in the districts where the program has been rolled out, many health centers are still collecting initial data on the 12 indicators and have not moved on to provide services. The success of the program is contingent on effective training, implementation, and regular follow-up, Human Rights Watch said.
Local community health centers have developed creative initiatives to support people with psychosocial disabilities. Puskesmas Cilandak in South Jakarta has created E-Mental, an Android-based application that allows community health workers to provide early intervention for people with psychosocial disabilities and support them in the community. Community health workers visit families to complete a simple 29-question survey to determine whether someone may benefit from psychosocial support and whether they need immediate assistance.
The program has reached 1,025 people, providing services in the community for 97 percent of them. Only one case was referred to a hospital. The app allows community health workers to systematically follow up with people and develop community-based support systems and coping mechanisms that do not rely exclusively on medication. Community health workers provide counseling, information on psychosocial support, and link people up to vocational training courses so they can become financially independent.
The Health Minister also created a mobile application to provide mental health information. As of July, the app had been downloaded 20,000 times, with 15,000 active users, according to government data.
People in Institutions
Under Indonesian law it is relatively easy to admit a person with a psychosocial disability to an institution against their will. In 2016, Human Rights Watch visited 16 institutions across the islands of Java and Sumatra and documented 65 cases of people arbitrarily detained in mental hospitals, government and private social care institutions, and faith healing centers. Two and a half years later, there has been little improvement.
Yayasan Bina Lestari Mandiri Brebes, a state-licensed Islamic healing center in Brebes, Central Java, which was described in the 2016 Human Rights Watch report, continues to chain people with psychosocial disabilities. In September 2018, all 50 residents of Bina Lestari were chained. People are chained for nearly 24 hours a day, unable to move more than two to four meters in any direction. They get no medical attention or mental health care, are given poor-quality food and are at risk of physical and sexual violence by other residents or staff.
The local Social Affairs department is aware that people with psychosocial disabilities are shackled at Yayasan Bina Lestari and at times they even send people there. The basis for admission and discharge is left entirely to the faith healer. The National Human Rights Commission conducted a monitoring visit to the institution in December 2017 but its report is yet to be made public.
Human Rights Watch also previously reported on the Yayasan Galuh Rehabilitation Center, a privately-run institution on the outskirts of Jakarta in Bekasi. It currently arbitrarily detains about 436 men, women, and children with psychosocial disabilities. People are brought to Galuh by their families or by local police if they are found living on the street. Unless the family comes to take the person out, they can remain there indefinitely.
Residents of Galuh also faced a range of neglect and abuse, involuntary treatment, seclusion, and restraint. They are forced to live in overcrowded and unsanitary conditions. They are held in close quarters without being able to go out or bathe regularly, which contributes to lice and scabies. Female residents are particularly at risk of sexual violence as the toilets have no doors and male staff oversee the female section. During the Human Rights Watch visit, male staff members observed as naked female residents bathed.
Ratih, a woman with a psychosocial disability who has been detained in Galuh for several years, said:
I have been chained here three times. The staff told me I was handcuffed for my own benefit. I got hit by the staff and was handcuffed for one whole week. I couldn’t even go to the toilet, I had to pee there, in my clothes. I had to ask my friend to help me eat but she was too scared…. I want to go home, I don’t belong here.
Recommendations
The Office of the Ombudsman, the National Human Rights Commission and the National Commission on Violence against Women should:
- Conduct regular, unannounced monitoring visits to government and private social care institutions as well as faith healing centers, with unhindered and confidential interaction with both staff and patients.
The Health Ministry should:
- Ensure that community-based mental health services work in partnership with organizations of people with psychosocial disabilities, their families, caregivers, and faith healers.
The Social Affairs Ministry should:
- Conduct regular, unannounced monitoring visits to government and private social care institutions as well as faith healing centers, with unhindered and confidential interaction with both staff and patients. The ministry should publicly report on their findings from these visits;
- Create and carry out a deinstitutionalization policy and a time-bound action plan, based on the values of equality, independence, and inclusion for people with disabilities. Preventing institutionalization should be an important part of this plan. The ministry should include people with disabilities and their representative organizations in developing the plan; and
- Engage spiritual leaders to challenge discriminatory beliefs and practices related to psychosocial disabilities to educate them about mental health and the needs of people with psychosocial disabilities.